Clinic visits for people with cystic fibrosis (CF) are time-consuming and expensive.
Not only are their appointments more regular than other patients – anything from once a fortnight to once every three months depending on their health – their nearest CF centre can be some distance away.
Up until now, a visit to hospital has been the only way for a clinical team to monitor their health. Not only is the process lengthy and exhausting, but there is potentially a lot of pressure riding on the appointment, too.
“Patients can come in for a routine check-up, but their results are so bad that we end up having to admit them to hospital as an inpatient,” explained Samantha Henman, Lead Cystic Fibrosis Nurse at Royal Papworth Hospital NHS Foundation Trust.
“That has a huge knock-on effect on their daily lives; they can’t go back home, they have to take unplanned time off work and their independence is suddenly gone. That creates a situation where CF patients get incredibly nervous and anxious before an appointment.”
Alternatively, patients can attend clinic but are completely stable and have needlessly wasted a day off work, school, or holiday.
However, a way of reducing the number of hospital visits for some CF patients is now being trialled in a first of its kind project at Royal Papworth Hospital, called Project Breathe.
Led by Professor Andres Floto, Project Breathe is funded by the UK CF Trust, the US CF Foundation, Microsoft, Magic Bullet and InnovateUK. It aims to evaluate whether we can use equipment and monitoring software to change the way that care for CF patients is managed.
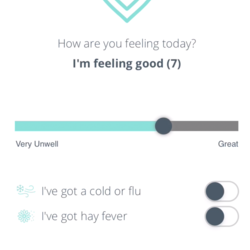
Once a suitable patient is identified for Project Breathe, they are supplied with the necessary equipment to take home, including; a lung function monitor; a saturation probe which measures the amount of oxygen in blood; a thermometer; scales; and a Fitbit which records data such as steps taken and resting heart rate and sleep.
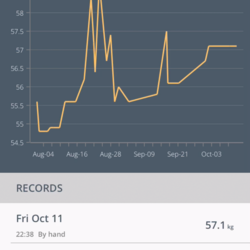
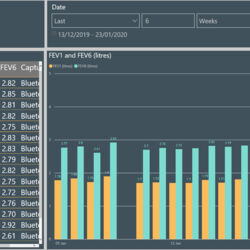
The data from these sensors is downloaded onto their phone and then sent to the patient’s dashboard which creates a picture of their health over time that both the patient and the hospital team can see.
The participants have also consented for their data to be analysed by machine learning experts (at the University of Cambridge and Microsoft Research) to develop early warning algorithms to detect the start of a clinical deterioration before patients are aware they’re becoming unwell.”
Project Breathe began recruiting in February 2019 and has now enrolled more than 80 patients from Royal Papworth Hospital, with plans to expand to other national and international CF centres after the first year.
“About a week to 10 days before a patient’s actual clinic I book a virtual clinic,” added Henman, “which involves me logging into the system and looking at the data they have been uploading. That is the virtual clinic.
“I’ll phone the patient and discuss their data alongside their symptoms. If everything looks stable, we then cancel their planned clinic and rebook for another date in the future. What this means is that we are in effect turning monthly visits into three-monthly for some patients and giving them more independence to see what their health is doing.
“It also takes away the pressure that you get with one-off measurements during a physical clinic, which captures very smalls bits of data at a specific time on a specific day. There are just so many positives.
“We hope that Project Breathe will improve patients’ experiences and improve their long-term health. It should allow for early detection and treatment of clinical deteriorations and also provide immediate feedback about the impact of starting or stopping particular therapies.
“Not only that, but it will reduce unnecessary hospital visits, minimising both disruption to their lives and the risk of cross-infection. It’s hopefully also going to have cost-savings for patients and hospitals.
“The end point of the first year of Project Breathe is to confirm that home monitoring and virtual clinics in an adult CF population are safe, verify the cost savings of that approach, and develop computer algorithms to predict exacerbations in a patient’s health.
“For year two and three we’ll be rolling Project Breathe out to other centres (in the UK and abroad) while we at Royal Papworth are trying out new software and sensors.”